A Diabetes Diagnosis: Learn How to Manage Your Condition and Blood Sugar with an Medication and Health Tracker App
If You’ve Been Diagnosed with Diabetes Type 2, You’ll Need to Change Your Lifestyle Habits, Track Your Blood Sugar, and Take Medication. Let MyTherapy Help You Implement These Changes and Ensure That You Adhere to Your Treatment
Type 2 diabetes is becoming increasingly prevalent and in the US alone, type 2 diabetes accounts for about 95% of all diagnosed cases of diabetes in adults. It is therefore the most common form of diabetes. 29,1 million people in the US have diabetes, but it is suggested that at least 8,1 million people may be unaware that they have it.
Unlike with diabetes type 1, people with type 2 diabetes produce insulin. However, the insulin (secreted by the pancreas) is either not enough or the body cannot recognize the insulin and use it effectively (this is known as insulin resistance). When there isn’t enough insulin, sugar (glucose)is unable to get into the body’s cells (for energy) and it builds up in the bloodstream instead, resulting in a high blood sugar level. If not treated properly, this can cause long-term health problems, such as kidney and eye damage, heart problems, and stroke.
In the early stages of the condition, a strict diet and exercise may be sufficient for keeping blood sugar levels within the normal (i.e. healthy) range. If this does not suffice, diabetic medications, such as Metformin, Januvia, Jardiance, and others, can help. If the condition continues to progress, insulin injections may also be required. If you have been diagnosed with diabetes type 2, it is important that you adhere to your treatment plan as strictly and responsibly as possible, as a high treatment compliance in the early stages of the condition can significantly reduce its progression. However, following a healthy lifestyle and taking medication regularly can prove difficult - especially when you have to change your daily habits. Smartphone apps, like MyTherapy, can offer you valuable support in this respect. Designed as an app for people with chronic conditions, MyTherapy will encourage you to adhere to treatment and help you make important lifestyle changes. It will also remind you to track your blood sugar levels and monitor your symptoms.
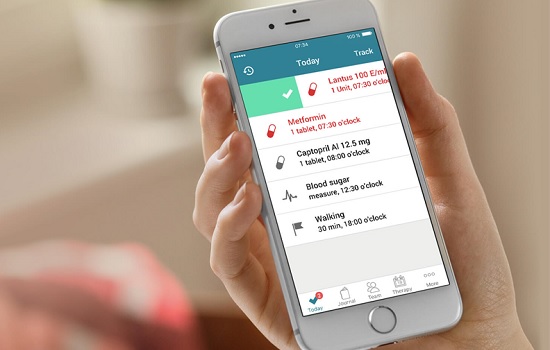
MyTherapy was designed for patients living with chronic conditions, like diabetes type 2. Similar to a personal health assistant, the app reminds you of important aspects of your treatment, such as taking your medication on time, exercising regularly, following a balanced diet, and tracking your blood sugar levels. The medication reminders help you take your daily medications on time and you can also use them to remind you of doctors’ appointments. All you have to do is log your data via the app's barcode scanner, built-in database, or manually - and the app will take care of the rest. It doesn’t matter how complex your regimen is - MyTherapy is designed to handle it.
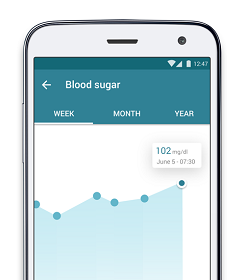
Apart from being a medication tracker, MyTherapy also comes with a built-in health diary that you can use to monitor your symptoms, blood sugar levels (before and after meals), medication side-effects, and other important measurements, such as weight, blood pressure, and weight circumference. You can also record any important lab results. With all these features, MyTherapy helps you lead a healthy lifestyle without having to think about it all day. MyTherapy even makes it easy to share data with your healthcare providers: the app generates monthly reports based on your logged data, which you can then share with your doctor either digitally or by means of a printout. This way, your GP or endocrinologist can quickly gain insight into how you’re doing and evaluate the effectiveness of your treatment.
Type 2: The Most Common Type
Type 2 diabetes is a metabolic condition that occurs when the body does not produce enough insulin or becomes resistant to insulin. Insulin is an important hormone that is produced by the pancreas. It helps the cells of the body take up glucose (sugar) from the blood so that it can be used as a source of energy. When there is a problem with insulin production, the cells don’t receive the sugar for energy (and begin to starve) and the sugar then begins to build up in the blood, resulting in high blood sugar levels. When the cells are starved, they begin to use other energy sources in the tissues, muscles, or organs. Over time, various complications can arise, such as kidney and eye damage, nerve damage, heart problems, and infertility. By definition, you will be diagnosed with diabetes if you have a blood glucose level that is greater than or equal to 126 milligrams per deciliter after an eight-hour fast.
Various factors contribute to the development of type 2 diabetes. They include:
- Genes: certain genes have been linked to an increased risk of developing type 2 diabetes. These genes affect the way the body makes insulin and can be passed on from parents and children.
- Lifestyle factors: you have an increased chance of developing diabetes type 2 if you have high blood pressure, are overweight or obese, are physically inactive, follow a poor diet, or have an increased waist circumference (where you carry extra weight around the middle, causing an ‘apple-shaped’ body).
- Cell dysfunctions: diabetes type 2 can also be caused by a cell dysfunction in the pancreas or by problems in cell signalling and regulation. For instance, it is possible that the liver, which usually produces and releases glucose, does not curb its glucose output after mealtimes when your blood sugar goes up by eating. This can cause excess glucose in the blood.
- Pre-diabetes: this means that your blood sugar level is higher than normal, but you don’t have diabetes yet. To remain pre-diabetic, you will have to implement strict lifestyle changes.
- Ethnicity: people are more likely to develop type 2 diabetes if they are Hispanic, African/ African-American, or Asian. Diabetes can be up to six times more common in these ethnicities.
- Age: the risk of type 2 diabetes increases with age. Usually diabetes type two affects people over the age of 40. This may be because people tend to gain weight and exercise less when they get older.
Signs and Symptoms to Look out For
The onset of diabetes type 2 is usually slow and symptoms can be mild at first. They include:
- Constant hunger and excessive thirst
- Lack of energy
- Unexplained weight loss
- Wounds and cuts that heal more slowly than usual
- Blurred vision
- Urinating more often than usual
- Itching around the genital areas or frequent episodes of thrush
Having type 2 diabetes means that the body is unable to keep blood sugar levels within a normal range. This means it is possible that people will experience episodes of extremely low blood sugar (hypoglycemia) and episodes of extremely high blood sugar (hyperglycemia). Symptoms of hypoglycemia include shaking, dizziness, and difficulties with speaking. Hyperglycemia causes frequent urination and increased thirst, among other things. Both can lead to unconsciousness if not treated.
If you experience any of these symptoms, you should go and see your doctor. He/ she will do a physical examination, as well as urine and blood tests to make a diagnosis. A common type of blood test is the glycated hemoglobin (HbA1c) test, which gives the average blood sugar levels over the past two or three months. This test is also used on people who have already been diagnosed with diabetes to determine how well their blood sugar is being controlled. Your doctor will also need to check that you don't actually have diabetes type 1. He/ she will do so by testing for autoantibodies and ketones in your blood. These are associated with type 1 diabetes, but not with type 2.
Treatment with Lifestyle Changes and Medication
Type 2 diabetes cannot be cured, but it is possible to control the symptoms and keep the blood sugar levels within a certain range. There are lots of treatment options available to help you manage your diabetes.
Often type 2 diabetes can be managed with behavioral changes and lifestyle changes. You will learn how to recognize when your blood sugar is too high or too low and what to do in these situations. In addition, you will be advised to include high-fiber foods, whole grains, and fruits and vegetables in your diet. You should also eat at regular intervals and exercise regularly, about half an hour of moderate-intensity aerobic activity (e.g. cycling or fast walking) a day.
If lifestyle changes are not enough to control blood sugar levels, medication might be necessary. There are several types of drugs which can help you with type 2 diabetes. They can cause various side effects and should only be taken after consulting your doctor. Medication for type two diabetes includes:
- Metformin can help you lower your blood sugar and improve your body’s response to insulin.
- Sulfonylureas (e.g. Glyburide, Glibenclamide) can increase your insulin production.
- Meglitinides or glinides (e.g. Starlix, Trazec, Novonorm, Prandin) are fast-acting medications that stimulate the insulin output of the pancreas.
- Thiazolidinediones (e.g. Anvandia, Actos) increase your body’s sensitivity to insulin.
- Dipeptidyl peptidase-4 inhibitors (also DDP4-inhibitors, e.g. Januvia, Janumet, Galvus, Jalra, or Trajenta) help reduce blood sugar levels.
- Glucagon-like peptide-1 receptor agonists (also GLP-1 receptor agonists, e.g. Byetta, Victoza) slow your digestion and improve your glucose levels.
- Sodium-glucose cotransporter-2 inhibitors (also SGLT2-inhibitors, e.g. Jardiance, Forxiga, Invokana, Suglat, Apleway) stop the kidneys from reabsorbing sugar back into the blood, meaning that more sugar is sent out through your urine.
If your body is unable to make enough insulin, then you may need insulin therapy. This can be in the form of insulin injections or an insulin pump.
Having type two diabetes increases the risk of developing heart disease, stroke, and kidney disease. Therefore, you may require additional medication if you are suffering from high blood pressure or high cholesterol levels.
MyTherapy: The App for Living Life with Diabetes Type 2
Type 2 diabetes can be well treated with lifestyle changes and adherence to a prescribed medication regimen. However, for diabetes medications to be effective, they need to be taken as intended - and this can be challenging in an everyday setting. MyTherapy is designed to help you with these adherence challenges. With its reminders (that can be used for anything from medication intake to taking a walk) and built-in digital health diary that lets you record symptoms, blood sugar levels, and other measurements; MyTherapy ensures that you get the best out of your treatment plan and encourages you to live a healthier, symptom-free life. The app even supports medications beyond diabetes so that you can manage all your pills and tablets in one place. And if you need some extra encouragement, you can invite friends and family on the app to help you with managing your diabetes effectively.