Hypertension is one of the most common diseases in the world, affecting millions each year. However, hypertension you have likely heard of, the standard high blood pressure condition, is not the only type of hypertension. Orthostatic hypertension and its low blood pressure counterpart, orthostatic hypotension are both widespread. An orthostatic, or postural, form of hypertension is one that occurs only when standing up from a seated or lying position. Given the variety of underlying causes and risk factors that can lead to the development of this condition, it is a great idea to understand key info such as what it is, how it’s diagnosed, what causes it, and how it’s treated.
What is Orthostatic Hypertension (Postural Hypertension)?
If you have heard of hypertension you probably already knew that orthostatic hypertension involved high blood-pressure. Orthostatic hypertension, also known as postural hypertension, is a less well-known form of hypertension that occurs abruptly when someone moves into an upright position. An increase in blood pressure of 20 mmHg or more when standing is the criteria for a diagnosis of orthostatic hypertension. This condition can pose serious problems as the sudden surge in blood pressure can lead to other life-threatening events such as heart attack, heart failure, stroke, or kidney failure. In severe cases of orthostatic hypertension, it can also result in patients experiencing the same typical symptoms that they would with hypertension. However, in the majority of patients with orthostatic hypertension symptoms are only present when the upright position is assumed.
What Are the Risk Factors and Causes of Orthostatic Hypertension?
Part of what makes orthostatic hypertension difficult to treat is the variety of underlying risk factors and causes that can lead to it. Many of the common risk factors are like those that are linked to hypertension. Age, medications, previous heat conditions, excessive heat exposure, bed rest, pregnancy, and heavy drinking all have been linked to the development of orthostatic hypertension. Aside from risk factors linked to the condition, several possible underlying causes have been identified. These are the most common:
- Dehydration – Dehydration typically does not lead to long-term orthostatic hypertension, but it can cause it in the short-term. Vomiting, fever, or just not drinking enough all can lead to experiencing symptoms of orthostatic hypertension. This is especially true in those who have had problems with high blood pressure in the past.
- Heart Problems – Heart conditions such as bradycardia or heart valve problems can lead to orthostatic hypertension since they prevent your body from responding fast enough upon standing up.
- Endocrine Conditions – Blood sugar problems are commonly linked to orthostatic hypertension. Additionally, adrenal insufficiency and diabetes can lead to the development of symptoms.
- Disorders of the Nervous System – Many diseases or disorders affecting the nervous system can potentially disrupt the body’s natural blood pressure regulation and lead to either orthostatic hypertension (or orthostatic hypotension).
How is Orthostatic Hypertension Diagnosed and Treated?
As briefly mentioned above, a rise in systolic blood pressure of 20 mmHg or more is considered to be the cutoff for diagnosing orthostatic hypertension. Oftentimes, doctors will utilize a tilt table test to make the diagnosis. A tilt table test, or TTT, involves laying a patient on their back on a special table while monitoring their blood pressure. The table then gradually tilts the patient into an upright position to see the observe the change in blood pressure. While it would be possible to just have a patient stand up while monitoring blood pressure, a tilt table test eliminates the possibility that the act of standing itself is what caused the change in pressure. It is the best test available to confirm that the upright position of the body is responsible for the change in blood pressure.
Unfortunately, there are no officially recommended treatments for orthostatic hypertension as there is still so little known about it and it can stem from so many different underlying causes. For the time being, treating patients with orthostatic hypertension comes down to trial and error. There has, so far, been some success treating patients by using the following drugs:
- Doxazosin – A drug commonly used to treat high blood pressure, doxazosin has been shown to be effective in reducing the effects of orthostatic hypertension. Treatment usually involves taking one dose (1-4mg) each night before bed.
- Carvedilol – Carvedilol is a beta-blocker commonly used to treat hypertension as well. While it has also been effective in treating patients, recent studies suggest that there is the danger of drug-induced postural hypotension (the opposite of hypertension) when patients are not in the upright position. This problem is not exclusive to carvedilol, but it has been the subject of more research recently.
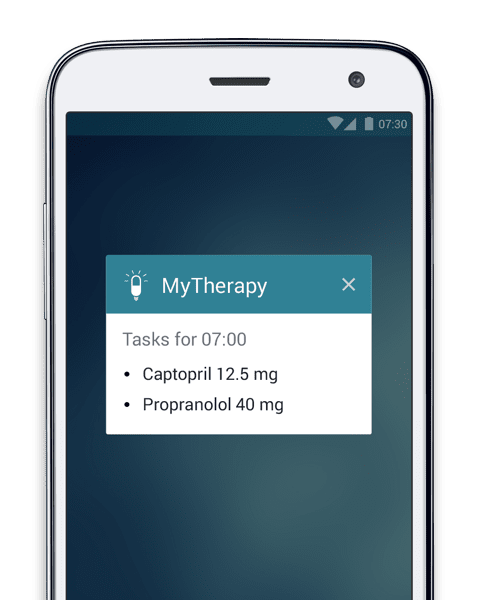
- Captopril – Captopril is another drug used for treating high blood pressure. It works by inhibiting the enzyme responsible for converting angiotensin I to angiotensin II. This in turn has been shown to reduce the effects of orthostatic hypertension when patients stand up.
- Propranolol Hydrochloride – Another medication used for treating orthostatic hypertension, propranolol is a beta-blocker also commonly prescribed to treat high blood pressure.
Aside from these medications, the treatment of coexisting conditions has also been shown to help in the treatment of orthostatic hypertension. One such condition is hypovolemia. Hypovolemia is a condition that results in reduced volume within the veins. This can come about because of losing both salt and water too quickly and affects the circulatory system adversely. In some cases, doctors have been able to treat hypovolemia with saline IVs and in turn, brought orthostatic hypertension back to a safe level.
Another method that has been used increasingly in recent years is exercise training. As is the case with hypertension, orthostatic hypertension effects can be lessened by maintaining good cardiovascular health. Some patients may find upright exercise difficult due to the symptoms of orthostatic hypertension. A great alternative can be cardio workouts that you can do horizontally. For instance, swimming or recumbent biking both provide great cardiovascular benefits without requiring any time spent in an upright position.
The final commonly used treatment is pressure garments. Pressure garments are worn in strategic areas of the body to regulate the movement of fluids, and in the case of orthostatic hypertension, reduce blood pooling. This has been effective in treating many patients but often has high rates of non-adherence due to issues of practicality. You can read more about how doctors use pressure garments to treat orthostatic hypertension here.
Here are some other articles we think you might be interested in:
This is How Tracking Blood Pressure at Home Can Help 103 Million Americans Living with Hypertension