What do citric fruits such as grapefruits, Seville oranges, and limes have in common with milk, aged cheeses, leafy greens, bananas, yogurt, and licorice? Aside from being delicious, of course, they all contain substances that can affect the way certain drugs behave. Such instances are called food-drug interactions, and the effects can range from minor to life-threatening. Similar drug interactions can happen with supplements and other medications. While that may sound daunting, there are a few simple steps you can take to mitigate the risk of drug interactions, so you can safely continue enjoying the foods you love, while reaping the health benefits supplements and medication offer. In this article, we explain the most common types of drug interactions, and provide a few useful tips to help you avoid them.
Food-Drug Interactions
Grapefruit: the forbidden fruit. At least, that is the case for people taking any of the dozens of drugs it is known to interact with. The Barbadian fruit contains a chemical compound that prevents an enzyme in the body from metabolizing certain drugs, including cholesterol-lowering statins such as simvastatin, leaving them free to reach potentially toxic levels. Other citric fruits, such as Seville oranges and limes, are also believed to decrease the body’s ability to absorb these drugs.
Calcium, found in dairy products including milk, yogurt, and cheese, can have a similar effect when it comes to absorbing tetracycline, an antibiotic used to treat a range of conditions.
Some cheese can also interact with monoamine oxidase inhibitors (MAOIs) – the very first class of antidepressant drugs. The Cheese Effect was discovered by a British pharmacist whose wife was taking a MAOI. He noticed that whenever she ate a meal containing cheese, she would suffer severe headaches. They were caused by the drug interacting with tyramine, an enzyme found predominantly in aged cheese. It was later found that the combination led to a hypertensive crisis – a dangerous spike in blood pressure that can lead to stroke.
When it comes to food-drug interactions, those taking warfarin – an anticoagulant (blood thinner) used to help those with conditions such as deep vein thrombosis and atrial fibrillation – must be particularly careful. The drug is known to react with dozens of foods, as well as supplements and other drugs. Vitamin K helps the blood clot – an important mechanism in the healing wounds – but the precise opposite of warfarin’s desired effect. Thus, vitamin K-rich foods such as cabbage, kale, and spinach can reduce the effectiveness of warfarin, increasing the risk of dangerous blood clots and stroke.
Supplement-Drug Interactions
Of course, while vitamin K is found in foods such as leafy greens, one may also take it in the form of a supplement and must be aware of the same interactions. The same is true of potassium. The brain, heart, and kidney are just three of the major organs potassium can help, making it a popular supplement. However, when taken in conjunction with angiotensin-converting-enzyme inhibitors (ACE inhibitors to you and me), used to treat high blood pressure, too much potassium has the potential to cause an irregular heartbeat, or heart palpitations. In extreme cases, this can be life-threatening.
As previously mentioned, warfarin is particularly susceptible to food-drug interactions, and the same is true when it comes to supplements. St. John’s wort, garlic, and ginseng are just a handful of the supplements that have been shown to interact with warfarin, and can lead to serious side effects such as bleeding and clotting issues.
Drug-Drug Interactions
Of course, drugs can also interact with one-another. While your doctor or pharmacist will likely check for drug interactions between prescription medications you take, the same checks may not automatically be in place for over-the-counter (OTC) medicines. Yet many OTC medicines can lead to harmful side-effects when combined with other drugs.
Nasal decongestants, which one may not think twice about taking to remedy a cold, can interact with MAOIs and hypertension medication, potentially causing a spike in blood pressure.
OTC antihistamines are also a go-to medicine for a range of minor health conditions, and can also raise the blood pressure of those also taking hypertension medication. As well as that, antihistamines may lead to excessive sleepiness and severely impaired concentration levels when take in conjunction with sedatives and tranquilizers.
Other posts you may be interested in on the MyTherapy blog:
- This is How Tracking Blood Pressure at Home Can Help 103 Million Americans Living with Hypertension
- Diabetes in the USA: Facts and Figures
5 Tips for Avoiding Drug Interactions
The risk of drug interactions increases with each and every medication you add to your regimen. Considering more than one in 10 Americans will have taken five or more medications in the last 30 days, it may seem like drug interactions are inevitable. However, with a few simple steps, even those with complicated treatment plans can limit the risk of drug interactions.
- Use the Same Pharmacy
There are automated systems in place to help flag, among other issues, drug interactions. For example, your insurance company may examine your claims to identify possible clashes. Similarly, chain pharmacies keep digital records that are easily checked at different branches. And, of course, pharmacies can contact one-another by phone, as well as your doctor, to gain information they do not have immediate access to. Nonetheless, such systems are not fault proof, so filling prescriptions – especially new ones – at the same pharmacy is the safest way of checking for possible interactions. It also allows you to build a relationship with your pharmacist, who will be the most knowledgeable person to speak to about drug interactions. - Understand Your Meds
When it comes to taking medications, there is no such thing as too much knowledge. When you leave the pharmacy with a new prescription, ask yourself: Do I know exactly what I’m taking, why, and how to do so? If the answer to any of these is anything other than a resounding ‘yes,’ the possibility of complications – such as drug interactions – is increased. The same questions should be applied to over-the-counter medication and supplements. If in doubt, ask your pharmacist. - Keep a Record
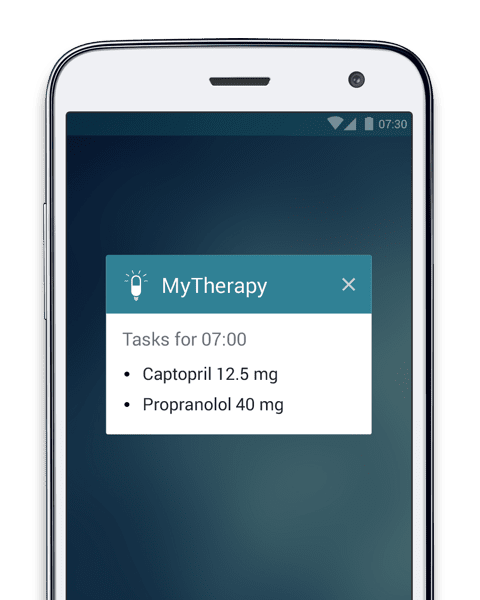
The more medications and supplements you add to your regimen, the more complicated it becomes, and the more susceptible you are to drug interactions. It is therefore worth keeping a record of exactly what you are taking, including prescription and over-the-counter meds, and supplements, all in one place. Your smartphone is the perfect tool for this, and one you will likely take with you anyway when you visit your doctor or pharmacy. MyTherapy (free for iOS and Android) allows you to set up your regimen – including OTC medicines and supplements – providing a comprehensive overview of your therapy. - Understand Food Interactions
While certain foods may interact with drugs, it does not necessarily mean you have to completely cut them out from your diet. The key is to understand the relationship between your food and drugs and know how you can avoid interactions. It may simply be a case of reducing your intake of a certain food, or allowing a period of time before or after taking your meds. As always, the more knowledge you arm yourself with, the better you can manage the relationship between your medications and the food you eat. - Beware of Alcohol
Alcohol is one of the biggest risk factors when it comes to drug interaction, with the potential to have an adverse effect when combined with hundreds of prescription and over-the-counter medications. This won’t be news to many, yet a study conducted by the National Institute of Health found that 42% of adults in the USA who drink regularly also take a medication known to adversely interact with it. While that doesn’t mean every case resulted in a potentially dangerous interaction, it is likely that there was an overlap in many cases. If you are unsure whether any medication or supplements you take interact with alcohol, speak to your pharmacist.
Complications caused by drug interactions may only be responsible for a small portion of the estimated $30 billion adverse drug reactions cost the US economy each year, but it is a portion that is avoidable with the implementation of a few simple safeguards. More importantly, such safeguards help ensure your medications work effectively, and mitigate the risk of potentially dangerous side-effects.
We hope the information in this article is useful. However, it should not be used as a substitute for professional advice. If you have any questions or concerns regarding drug interactions, speak to your pharmacist, doctor, or healthcare professional.
For more information about drug interactions, visit the FDA website
Take a look at some of the other posts on the MyTherapy blog: