Rheumatoid arthritis (RA) is a chronic disorder that attacks joints. The pain and stiffness of joints occur suddenly, develop quickly, and can hinder an individual’s ability to do daily activities. There is still no cure for RA. Fortunately, in the last few years a new class of biological medications (also known as ‘biologic medications’ or ‘biologics’) has been developed and has greatly improved the outcomes of RA treatments. Just like any other drug, including the conventional RA medications, this biological therapy comes with potential benefits and potential adverse side effects. In this article, we’ll discuss the available medications for RA, the differences between the conventional and recently developed treatments, and help you answer the question, “which treatment is right for me?”
Definition, symptoms, and causes of rheumatoid arthritis
RA is an auto-immune disorder that generates pain, swelling, and stiffness in joints. This condition occurs because the immune system doesn’t work properly and starts to attack the healthy joint tissues. Consequently, your joints are inflamed and can cause chronic pain, lack of balance, and deformity.
The symptoms of RA often happen suddenly, and the condition can worsen quickly. Normally, the pain starts in the small joints in the hands and feet (fingers and toes) before developing in other joints (wrists, ankles, and knees). Both sides of the body are usually affected at the same time and to the same extent, but this doesn’t always happen. Some people also experience stiffness, particularly in the morning right after you wake up or after sitting/lying still for a long time.
If you often feel tired, have a poor appetite, and experiencing weight loss along with the conditions mentioned before, you should be alert and check yourself to a doctor. Early diagnosis and intensive treatment for RA are important. The sooner you get the treatment, the more effective it’s likely to be. The previously mentioned symptoms are not a comprehensive list of all RA symptoms. Please confer with a medical practitioner for an accurate diagnosis.
Additionally, RA is three times more likely to occur in women than men and can affect anyone of any age, although typically the symptoms start between the ages of 30 and 60. The exact causes of RA are still unknown, but many believe besides sex and age, having a family member with RA or smoking can increase the odds of developing this disease.
Treatments for rheumatoid arthritis
The main treatment goal of RA is to control the inflammation in the joints, ease pain, prevent/slow down damage, and ultimately reduce disability linked to RA so that people who live with RA can be as active as possible.
RA medications are often divided into four main types: nonsteroidal anti-inflammatory drugs (NSAIDs), steroids, disease-modifying anti-rheumatic drugs (DMARDs), and biological treatments (bDMARDs). The first three drug types are typically administered orally, and the last type is either through injection or infusion. Each drug type has different purposes in treating RA and can’t simply be switched, replaced, or combined with other types.
1. Nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs aid to relieve pain (like painkillers) while also reducing inflammation in the joints. Thus, they only lessen the pain and not stopping RA from getting worse. If you have moderate to severe RA, your doctor is likely to prescribe you other drugs to prevent further joint damage.
Depending on the patients’ condition, some people may be prescribed over-the-counter NSAIDs, such as ibuprofen (Advil and Motrin IB), and some may need a prescription version of NSAIDs, such as celecoxib (Celebrex). The prescription version of NSAIDs requires fewer doses as it offers a higher dose with longer-lasting results.
Side effects:
Side effects of taking NSAIDs are uncommon to occur but can include heart problems, kidney damage, and stomach irritations. You may also be given another medicine along with NSAIDs, such as a proton pump inhibitor (PPI), to reduce the amount of acid in your stomach and lessen the risk of damaging your stomach lining. Consult with your doctor to consider the benefits of NSAIDs against the possible risks.
2. Steroids
Steroids are powerful medications to reduce pain, stiffness, and inflammation. Depending on the level of the severity, your doctor may recommend taking this medication for a longer time to control the pain and inflammation before gradually tapering off the dosage.
Some common steroids for RA are prednisone (Deltasone), hydrocortisone (Cortef), and methylprednisolone (Medrol). They can be given as a tablet or an injection either directly into an inflamed joint or into a muscle.
Side effects:
Broadly speaking, taking steroids in lower doses for a shorter time means fewer side effects. Some of the side effects of steroids may include weight gain, osteoporosis (bone loss), diabetes, and hypertension, among others.
3. Disease-modifying anti-rheumatic drugs (DMARDs)
DMARDs are usually given at the beginning of your treatment. These medications work by altering the underlying disease rather than treating symptoms by blocking the effects of the chemicals released when your immune systems attack your healthy joints. In this way, further damage to your bones, tendons, and ligaments can be held back.
DMARDs can take weeks or even months to show their effects. The typical prescription of DMARDs for RA is methotrexate (Trexall). If that alone doesn’t reduce the inflammation, you may be asked to try other types of DMARD such as hydroxychloroquine (Plaquenil), leflunomide (Arava), sulfasalazine (Azulfidine), or tofacitinib (Xeljanz). Once you find the most suitable DMARD, you’re likely to take this medicine long term.
Side effects:
Side effects of DMARDs vary from mild responses (such as feeling sick, loss of appetite, and headaches), to something more serious (such as severe lung infections, liver damage, and bone marrow suppression). You may have to take regular blood tests, X-rays, and a breathing test to monitor the latter group of side effects, but most people tolerate DMARDs well.
4. Biological therapies (bDMARDs)
Biological therapies are a newer form of RA treatment that belongs to the DMARDs drug class. Thus, some also called it biologic(al) DMARDs (bDMARDs). They are built from genetically engineered proteins called anti-TNF drugs that target different parts of the immune system to stop them from attacking your joints. In this way, the drugs tend to work more quickly than the conventional DMARDs in decreasing joint inflammation and tissue damage.
Biological DMARD treatment is usually given in combination with non-biological DMARD medications (such as methotrexate), or when the non-biological DMARD medications aren’t responding well to you. This latest protein-engineered treatment comes in the form of injection or infusion. Some of the biological drugs include abatacept (Orencia), adalimumab (Humira), and anakinra (Kineret), among many others.
Side effects:
Since the biological DMARDs slow down your immune system, consuming this type of drug can also increase infection risks. You may feel sick, have a high temperature, and headaches. In some cases, taking biologicals can also increase the risk of blood clots in the lungs, tuberculosis, and cause trouble breathing.
The list above isn’t a complete list of all possible effects of taking RA medications. Talk with your doctor to find out what’s the best treatment for you and the side effects that may occur.
Conventional (DMARDs) vs biological therapies (bDMARDs)
Although bDMARD is the new class drug that stems from DMARDs, it has several differences.
- Effectiveness - bDMARDs are believed to be more effective in treating RA than other drug types, including DMARDs. However, just like other RA medications, they can’t cure RA. bDMARDs can only slow down RA progressions.
- Cost - bDMARDs are more expensive than DMARDs or other RA drug types. It can cost upwards of $45,000 annually for the infusions. Check your insurance plan to see whether it covers this medication before deciding which type to get.
- Response time - some of the bDMARDs may work fairly quickly, but each patient has a different response time.
- Types of administration – bDMARDs are given by injection or infusion. If you’re prescribed the injectable bDMARDs, such as adalimumab (Humira), you have the possibility to administer it yourself at home. If you’re prescribed the infusion bDMARDs, such as infliximab (Remicade), you have to go to a hospital or an infusion clinic. The infusion time may take between 15 minutes and four hours or more, depending on the medication you receive. If the idea of self-injection or getting your hand/arm hooked to an IV is daunting, you can talk to your doctor about your concerns and discuss other medication possibilities.
- Side effects – since bDMARDs are administered through injections or infusions, they could cause skin reactions at the site of the injections, such as redness, itching, pain, and swelling. On the other hand, because bDMARDs works by targeting specific parts of the immune system, it is likely to cause fewer side effects than other types of drugs. However, side effects, such as blood clots and difficulty in breathing, are still possible to occur. Tell your doctor about any (unusual) symptoms that you may experience after treatment. Keep in mind that everyone reacts differently even if they’re given the same drug.
- Not for everyone - biological medications may cause a dormant infection, such as tuberculosis and hepatitis, to become active again. For this reason, you may have to take some tests before taking one of the bDMARD drugs. Please note that not all health conditions that can interfere with biological therapy are mentioned here. To avoid any unwanted effects, you should discuss your health history with your doctor.
Conclusion: Which therapy is right for me?
Determining the right therapy for you depends greatly on your condition. Each drug/treatment type has its own purposes (relieving pain, reducing inflammation, and stopping immune system attacks on joints), and each patient has a unique condition. If you’ve been diagnosed with RA, usually you’ll be prescribed oral medications as a starter. If your condition isn’t progressively improving, injection or infusion may substantially help with the progress. You may have to try several medications before finding the one that is right for you. A combination of two or more treatments is also common in treating RA.
As for choosing between conventional (DMARDs) or biological treatment (bDMARDs), besides taking your RA condition into account, the cost, routes of administration, and your medical history can also play a role in assigning the medications. Consult with your doctor, check your health insurance coverage, and ask yourself whether having an injection or infusion is tolerable. You and your doctor can decide which therapy fits your condition the most. Remember, with proper treatment, you can lead a full and active life even if you experience RA.
Here are some other articles we think you might like:
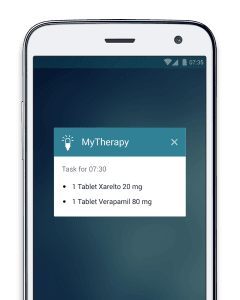
Living Well with Rheumatoid Arthritis: 3 Apps You Can Download Today