Multiple sclerosis (MS) is a mystery gradually being unravelled by research aimed at discovering the underlying cause of the disease, a reliable test to diagnose it, and, of course, a cure. Since French neurologist, Jean-Martin Charcot, first identified ‘sclerose en plaques’ in the 19th Century, our understanding of MS has significantly improved, leading to better diagnostic and treatment methods. However, while progress continues to be made, certain myths and misconceptions can be hard to shift. Here are a few common myths about MS, and the facts behind them.
Multiple Sclerosis Myths & Facts – Bitesize
❌ Multiple Sclerosis Always Leads to Severe Disability
✔️ Walking aids are common for people with MS, but often used occasionally for added accessibility. Wheelchairs are less common and, again, often used intermittently
❌ Multiple Sclerosis Affects Everyone in the Same Way
✔️ There are four main types of MS, all of which progress differently. Even in those with the same form of MS, it is a hugely variable disease with differing symptoms
❌ Multiple Sclerosis is a Terminal Illness
✔️ MS is rarely fatal. Life expectancy is 5-10 years below the general population, and the gap is decreasing all the time
❌ ‘Liberation Treatment’ Can Treat Multiple Sclerosis
✔️ Despite huge publicity, there is no evidence that Dr. Zamboni’s liberation treatment is effective in treating MS
Keep reading to learn about each myth and fact in more detail
Myth: Multiple Sclerosis Always Leads to Severe Disability
“I don’t want to end up in a wheelchair.”
This sentence, or a variation of it, is often at the forefront of one’s mind when diagnosed with multiple sclerosis. There is no denying that MS can be a debilitating disease, and one that can result in the need for walking aids or wheelchairs. However, thanks to medical advancements in the last two and a half decades, it is wrong to assume that this is a guaranteed prognosis.
While Professor Charcot may have made the link between the plaques in the brain and spinal cord and the symptoms of MS in 1868, he was at a loss when it came to treating it. This is no slight against him, though, as no effective treatment existed for the following 125 years. During that time, research helped answer questions about the progression of symptoms and the underlying mechanisms of the disease. It wasn’t until the 1960s that the possibility of MS being an autoimmune disease – the most widely accepted theory today – was considered.
Understanding the mechanisms of MS has helped doctors diagnose the disease earlier, as have medical innovations. The invention of magnetic resonance imaging (MRI), for example, helps identify damage of the central nervous system, one of the key criteria in diagnosing MS.
The practical benefits of over a century of research came to the fore in the early 1990s, when drugs capable of altering the progression of MS were made available.
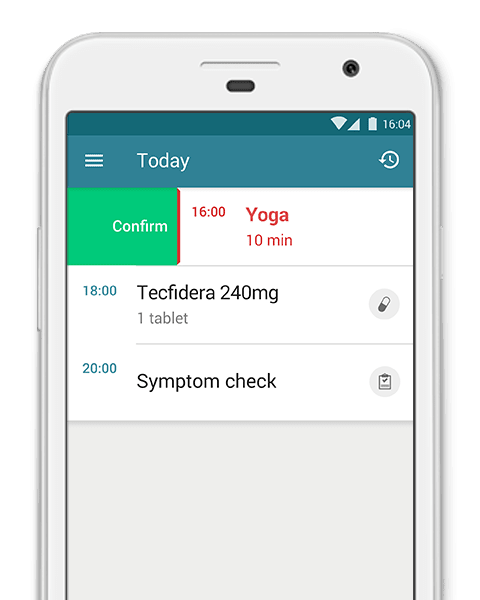
Since then, our understanding of the pathogenesis of MS has continued to improve, and this understanding has led to significant advancements in treatment. The specific therapy prescribed to an individual depends on a multitude of factors: the form of MS one is diagnosed with, severity, other health issues, and treatment history being but a few. Regardless of one’s particular circumstances, there are now a range of treatment options to be explored, with at least a dozen disease-modifying therapies available in most countries, so the chances of finding one that slows the progression of MS is higher than ever.
Of course, despite phenomenal advancements in MS treatment, walking aids and wheelchairs are still a possible outcome for many people. While it is impossible to know exactly the percentage of people with MS who use such tools, many who do use them need only do so sporadically. For many, occasional use of walking aids and wheelchairs opens up a world of possibilities that would otherwise have been inaccessible.
Regardless, the idea that MS inevitably leads to severe disability – and thus the need for permanent walking aids or wheelchair use – is most certainly a myth.
Myth: Multiple Sclerosis Affects Everyone in the Same Way
This is largely linked to the myth that everyone with multiple sclerosis is destined to require walking aids and the use of a wheelchair. The misconception is that once one is diagnosed with MS, the disease will progress in a very particular way.
This simply is not the case. Firstly, there are four main types of MS, all of which have different characteristics. As explained in our blog, Multiple Sclerosis Q&A, they are:
- Relapsing-Remitting MS (RRMS): the most common type of MS, accounting for over 80% of patients. Symptoms can remain dormant for years, even if the disease is fundamentally active. Relapses are unpredictable; new and existing symptoms can occur suddenly, lasting a few days or weeks, before regressing
- Secondary-Progressive MS (SPMS): often considered the second stage of the disease, 40% of those with RRMS progress to SPMS within 10 years. Relapses occur as in RRMS, but do not regress to the same extent, and symptoms gradually worsen between them
- Primary-Progressive MS (PPMS): affecting approximately 10% of MS patients, PPMS is relatively rare. Those with it do not have relapses and regressions like the aforementioned types. Rather, symptoms gradually worsen from the outset, although temporary improvement can occur
- Progressive-Relapsing MS (PRMS): affecting roughly 5% of patients, PRMS is the least common type of MS, and characterised by a steady worsening of the disease, along with relapses, but no remissions
As you can see, the course MS takes is highly dependent on the form one lives with. Even then, the progress and severity of MS cannot be assumed simply based on the type of MS, nor can each individual’s response to drugs capable to altering the disease course.
There is similar unpredictability when it comes to symptoms, which vary greatly depending on the particular nerve cells damaged by the disease – which is seemingly random. According to the National MS Society, common symptoms include, but are not limited to:
- Fatigue
- Walking difficulties
- Numbness and tingling
- Vision problems
- Cognitive changes
Less common symptoms include:
- Speech problems
- Tremors
- Hearing loss
These are just a handful of the symptoms that are associated with MS. However, as MS damages nerve cells, and nerve cells carry electrical impulses that control practically everything we do, the list of possible symptoms is endless. Robert Joyce, who blogs about his life with MS and was a guest author on this blog, has had a chronic headache from the moment a car crash in 2014 reignited his MS, the symptoms of which had been dormant for a decade. This is just one example of an unexpected, unpredictable, and severe symptom.
Robert’s full story about his life with MS can be found here:
Richard, who moved around the world after being diagnosed with MS, also shared his story with us:
- Traveling with MS: My Journey from America to Bali - Part One of Two by Richard Boughton
Essentially, there are three key variables when it comes to how MS affects each individual: the type of MS; one’s response to different treatments; the specific nerve cells damaged. Even with each variable considered, MS is still a wildly unpredictable disease, and the progression, severity, and symptoms will vary with each individual case.
Myth: Multiple Sclerosis is a Terminal Illness
There is a rare form of multiple sclerosis (called *Marburg acute multiple sclerosis*) that can fit this description, but it is certainly not the norm. The National MS Society say life expectancy of someone with MS is seven years less than the general population, an estimation mirrored by the NHS , who have the figure at five to 10 years. Both organizations point out that the gap is closing all the time. As treatment options continue to advance, a diagnosis of MS will likely have a declining effect on life expectancy.
Clearly, then, MS is not normally a disease “that cannot be adequately treated and is reasonably expected to result in the death of the patient within a short period of time.”
Multiple sclerosis is, however, both a chronic disease (lasting more than three months) and a lifelong disease, as there is not currently a cure. Considering terms such as ‘terminal,’ ‘chronic,’ and ‘lifelong’ are sometimes used incorrectly or interchangeably, it is easy to understand why confusion occurs.
It is also important to understand that while MS is not a fatal illness, it can have fatal consequences. People living with MS are believed to be at greater risk of cardiovascular diseases or respiratory problems, as well chest and bladder infections that can be dangerous when not promptly treated.
MS is many things, and the terminology can be confusing at times, but the common misconception that it is a terminal illness is one that can be laid to rest.
Myth: ‘Liberation Treatment’ Can Treat Multiple Sclerosis
The term chronic cerebrospinal venous insufficiency (CCSVI) burst on to the scene in 2009, thanks to Dr. Paolo Zamboni from the University of Ferrera in Italy, who claimed it was a possible cause of multiple sclerosis. Dr. Zamboni, whose wife lives with MS, theorized that the underlying cause of the disease was a narrowing of veins in the neck and head – a phenomenon he labelled CCSVI. This narrowing, his theory suggests, restricts blood flow and causes a series of events that eventually triggers the immune system to attack the fatty tissue protecting your nerve cells, called the myelin sheath.
The immune system destroying the myelin sheath has been widely recognized as the cause of MS for decades, but it is not understood why it does so. The fact Dr. Zamboni’s theory gave an explanation is what separated it from other theories regarding the mechanisms of MS.
What also separated it – and helped generate a massive amount of publicity – was that Dr. Zamboni claimed to have a highly effective therapy: liberation treatment. If narrow veins were the root cause of MS, widening them would be the obvious solution, and this is exactly the treatment Dr. Zamboni advocated. Furthermore, he published a study that appeared to show positive results of such treatment – which involves using a tiny balloon to open or widen the vein.
Naturally, this garnered media attention and sent a wave of optimism throughout the MS community. However, it was also met with scepticism from experts within the field, who doubted the theory and were critical of the methods used in Dr. Zamboni’s study, citing a lack of a control group as a particular concern.
Since then, CCSVI has been a highly controversial topic. On the one hand, you have people living with MS who saw a potentially life-changing treatment; on the other hand, there was a medical community and government organizations demanding further scrutinization. Countless studies have subsequently been performed and millions of dollars have been spent investigating CCSVI, its connection to MS, and the effectiveness of liberation treatment.
The consensus, unfortunately, is that it is ineffective. That was the conclusion of a study performed by the University of British Colombia in Canada, the country with the highest prevalence of MS in the world and where demand for CCSVI was greatest, and a recent study performed by Dr. Zamboni himself. The study concludes that the treatment “has proven to be a safe but largely ineffective technique; the treatment cannot be recommended in patients with MS.”
CCSVI is still a widely debated topic. However, in the near-decade since it first received public attention, the vast majority of experts are in agreement that Dr. Zamboni’s theory does not stand up to scrutiny. With Dr. Zamboni himself conceding that liberation treatment is ineffective, it is safe to file this one in the ‘myth’ category.
It has been 150 years since Professor Charcot identified ‘sclerose en plaques.’ While a cure is still yet to be discovered, the tireless research performed in that time – and still being performed around the globe today – has helped debunk a few myths and misconceptions about multiple sclerosis.
Continuation of such research will no doubt answer many of the questions that still remain.
If you would like to read more about MS, check out these other posts on the MyTherapy blog: